Common causes of abdominal muscle pain
The most common situation is pain in the abdominal muscles associated with natural physiological causes: overexertion, sports, sudden stretching. However, there are also pathological factors that lead to discomfort:
- Stretching of organ walls. Pain in this area may result from an increase in the size of the stomach, intestines and arteries. These processes occur not due to overeating, but due to dangerous pathological processes, as well as during pregnancy in women. Symptoms of organ stretching affect only smooth muscles, and the pain is called visceral.
- Mechanical damage to muscle tissue. If there is a strong blow to something, or a person is pierced with a sharp object, the muscle tissue tears, swells, and pain appears.
- Psychological disorders. Some people experience muscle pain as a result of stress and overexertion.
- Dysbacteriosis. One of the reasons for the increase in intestinal size. With dysbacteriosis, the organ becomes greatly stretched, symptoms such as constipation or diarrhea appear, the temperature rises, and nausea occurs.
If you have chronic diseases, you can suspect their exacerbation when pain appears in the rectus or oblique abdominal muscles.
Causes of damage to muscle structures
In general, ruptures and sprains of muscle structures belong to the same class of injuries and differ only in severity. Thus, classic sprains correspond to mild forms of the pathological process, in which only individual fibers of soft structures are susceptible to damage. At the same time, muscle ruptures can be partial or complete.
Among women
As practice shows, quite often in pregnant women in the last stages of gestation, also during childbirth, the muscles can be damaged accordingly, forming partial tears. Such spontaneous pathologies primarily manifest themselves in women in the muscles of the lower section (lower abdomen) pyramidal and rectus.
In addition to the above reasons, direct injuries to soft fibers as a result of strong physical impact, overexertion, usually against the background of insufficient muscle development, are also considered classic predisposing circumstances.
In men
In representatives of the stronger sex, it is often quite difficult to visually identify a specific type of injury to the abdominal muscle.
During pregnancy and after childbirth
Most often, sprains or ruptures of the abdominal muscles in women after childbirth and during their process are formed when the expelled fetus ceases to exert pressure from the inside and the corresponding structures contract extremely quickly. Surgical intervention, for example, caesarean section, with the formation of a number of complications, also has a pathological effect.
Pathologies that provoke myalgia
Myalgia is pain in muscle tissue, which is accompanied by spasms. Among the most common diseases that cause myalgia in the rectus and oblique abdominal muscles are:
- pathologies associated with metabolism - diabetes, gout, metabolic syndrome;
- viral infections – for many people, one of the first symptoms during the flu is muscle pain;
- vascular disorders, including aortic aneurysm.
However, myalgia can also be triggered by such trivial factors as prolonged stay in an uncomfortable position.
Myalgia can be distinguished from simple tension by such a sign as long-term persistence of pain. The symptoms in this case do not go away after rest, as they are associated with more serious processes. With myalgia, a burning sensation, nausea, and chills often occur.
Myositis as a form of myalgia
Myositis is an inflammation that occurs in skeletal muscles. One of the most serious forms of myalgia, which can be associated with serious diseases of the musculoskeletal system. But in some cases, myositis develops as a result of ARVI, tonsillitis, or with excessive physical exertion.
Some forms of myositis are thought to develop due to exposure to bacteria and toxins. This condition can be caused by abuse of alcohol, cocaine, and certain medications (statins, interferons, colchicine).
With myositis, a purulent process begins in the muscles, associated with chronic infections in the abdominal cavity. Symptoms rarely affect only the abdomen: not only the external oblique muscle hurts, but also the fibers of the neck, lower back, lower leg and chest. Myositis is accompanied by swelling, fever, fever and headaches.
Causes of muscle pain not associated with myositis
Acute muscle tension can occur in the following conditions when the abdominal wall becomes hard:
- inflammation of the appendix - pain is usually located on the right in the iliac region;
- intestinal obstruction – combined with symptoms of acute intoxication, accompanied by prolonged constipation and a strong increase in the size of the abdomen;
- perforation of the ulcer - acute dagger pain is associated with gastric bleeding, blood is present in the vomit and stool;
- vascular accidents - infarction of the intestines and other organs, thrombosis;
- acute cholecystitis - pain is located on the right hypochondrium, requires immediate surgical assistance;
- acute pancreatitis - symptoms are similar to cholecystitis, but the pain can be localized on the left;
- rupture of the fallopian tube during an ectopic pregnancy - the woman’s well-being rapidly deteriorates;
- rupture of an abdominal aortic aneurysm - a person feels acute diffuse pain;
- inflammation of the ovaries or uterus - endometritis, adnexitis, as well as hemorrhage in the ovary.
All these pathologies require immediate surgical care - when the first signs appear, you should consult a doctor. These symptoms are usually distinguished by unbearable pain, pallor, vomiting and nausea, fainting and bloody discharge in women.
Other conditions in which pain in the rectus abdominis muscles are severe include: strangulation of an umbilical or inguinal hernia, acute strain of the muscles of the anterior abdominal wall as a result of lifting heavy objects or injuries. Similar symptoms can be observed in people with diseases of the spine: tuberculosis, spondylolisthesis, osteochondrosis, trauma.
Features of pain during pregnancy
In pregnant women, constant pain in the oblique or rectus abdominal muscles may be associated with some serious abnormalities:
- Placental abruption. The pain is severe, localized at the bottom, often combined with bleeding and watery discharge. There is a high risk of fetal death as a result of hypoxia.
- Risk of miscarriage. The pain is combined with small amounts of blood, and a pulling sensation appears in the lower back.
- Ectopic pregnancy. The pain is very strong, radiating to the groin and back, the symptoms are localized on the left or right side - depending on where the egg is implanted.
- Digestive system disorders. Due to compression of the intestines and stomach by the growing fetus, constipation, flatulence, and bloating often occur.
- Stretching the abdominal muscles. This is a normal process that intensifies in the 3rd trimester.
Also, in women during pregnancy, chronic diseases worsen, pathologies of the pancreas, bile, and intestines arise, and appendicitis appears.
Diastasis
Diastasis occurs when the linea alba (the junction of the broad muscles) separates. The reasons are pregnancy and childbirth, heredity or obesity. Diastasis recti can occur in men and children.
During pregnancy, the connective tissue between the vastus muscles becomes loose so that the belly can expand. After childbirth, the tissue itself strengthens and the shape of the abdomen is restored within a year. But if a woman works hard on her abs or lifts weights, the tissue does not contract.
Pathology appears with obesity or sudden weight loss, when the connective tissue does not have time to contract, which leads to its “excess”. Muscle divergence also causes an increase in intra-abdominal pressure, for example, a hacking cough, heavy lifting, constipation, or playing sports.
With dysplasia, the structure of ligaments and tendons is disrupted, which leads to excessive extensibility of the connective tissue and provokes the occurrence of diastasis or the formation of hernias. Pain in the abdominal muscle fibers when impaired can vary in nature, strength and duration. The pain often intensifies with prolonged walking, physical activity, and heavy lifting.
With diastasis, muscle fibers are weakened and do not perform their function, so pain can appear even with little physical activity. Due to improper distribution of the load, internal organs may become mixed up, an umbilical hernia may form, digestion problems may occur, and pain in the spine may occur.
If your abdominal muscles hurt due to exercise, no special treatment is required, since the symptom will go away on its own in 1-2 days. You can reduce pain by doing a massage or taking a contrast shower. Tension of the abdominal muscles is one of the symptoms of an “acute abdomen”, which requires surgical intervention.
Therefore, if your abdominal muscles hurt severely for no reason (you have not previously engaged in physical labor or exercise), and there are other symptoms, for example, nausea, general weakness, fever, abnormal bowel movements, then you need to seek medical help. Only after finding out the causes of long-term or periodic muscle pain can you understand what needs to be done to eliminate them.
Muscle pain is a normal condition after physical activity. But it happens that the rectus or internal oblique abdominal muscle hurts for no apparent reason. And if you look closely, you can find additional symptoms of an unpleasant condition, indicating the development of certain diseases.
Methods of diagnosis and treatment for muscle pain
Diagnosis of pain in the abdominal muscles occurs in several stages. The first is palpation. The doctor determines the condition of the abdominal wall. Next, they take blood and urine tests, and also do an ultrasound. In some cases, x-rays and an ECG are required.
Treatment methods depend on the type of disease. Gynecological disorders are treated by a gynecologist; for gastrointestinal diseases, therapy is prescribed by a gastroenterologist. In acute conditions, surgical intervention is often required, followed by antibacterial therapy: removal of a ruptured ovary and fallopian tube, elimination of an inflamed appendix.
Symptomatic therapy includes taking antispasmodics, NSAIDs, probiotics, and anti-inflammatory drugs when necessary. Be sure to prescribe a gentle diet to avoid unnecessary stress on the internal organs.
To prevent pain, it is important to monitor your health and treat chronic diseases in a timely manner. You should not overexert yourself when playing sports; you should always warm up before training. To prevent pain from appearing, you need to train different muscle groups on different days.
source
What to do if your muscles hurt a lot after training?
In order to at least slightly reduce the pain after playing sports, you need to do another workout, but with less strength loads. During training, you should not do more than you can realistically do. First of all, evaluate your capabilities, and then you can begin to gradually increase the load. And don't forget to stretch before and after your workout. Stretching will help you in the fight against sore throat, and can also prevent its occurrence. Another option is to use a warm shower or bath. And for a relaxing effect, you can add a couple of drops of essential oil and get maximum pleasure from it.
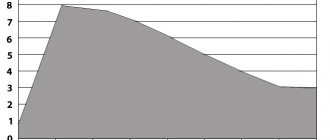
Spread of pain from the rectus abdominis muscle
Myofascial trigger points located in the abdominal muscles may present with referred pain, which can be difficult to diagnose. False visceral pain, manifested from myofascial trigger points embedded in the abdominal muscles, can arise not only in the same segment of the abdominal wall; in addition, it can also radiate to the back. Painful sensations caused by trigger points are often accompanied by somatovisceral reactions, in the form of violent vomiting, nausea, loss of appetite, intestinal colic, loose stools, spasm of the sphincters and bladder, and menstrual irregularities. Such symptoms, accompanied by abdominal pain, may resemble acute diseases of the internal organs, for example, cholecystitis or appendicitis.
The rectus abdominis muscle is attached inferiorly along the crest of the pubic bone, with intertwining fibers at the level of the symphysis.
At the top, the rectus abdominis muscle is attached to the cartilages of the ribs V, VI and VII. The fibers of this muscle are interrupted by three or four transverse tendinous septa, one of the three permanent septa located near the apex of the xiphoid process, another at the level of the umbilicus, and the third septum located midway between them. In some cases, there are also one or two bridges, partially formed, and they are located below the navel. The fibers of the upper rectus abdominis muscle can sometimes overlap the abdominal portion of the pectoralis major muscle, which can cause pain caused by myofascial trigger points in this area and radiating down the front of the chest. The functions of the abdominal muscles are aimed mainly at increasing intra-abdominal pressure, flexion and rotation of the spine. The rectus abdominis muscle is the primary mover, providing flexion of the lower thoracic and lumbar spine. The rectus abdominis muscle is largely involved in the tension of the anterior abdominal wall, thereby causing an increase in intra-abdominal pressure.
A single group of muscles of the abdominal wall of the abdomen is involved in the implementation of rapid and complete exhalation during rapid breathing, helping to drive blood from the veins of the abdomen to the heart. When the abdominal wall relaxes at the moment of inhalation, blood flow in the abdominal veins increases, which stimulates the outflow of blood from the lower extremities.
When exhaling, in the absence of pathology of the valves of the veins of the lower extremities, the muscles of the abdominal wall contract and the blood tends upward to the heart.
The rectus abdominis muscle responds during walking to each step cycle during walking.
The rectus abdominis muscle is actively involved during a jump at the moment the feet lift off the support, but is not always active when landing.
When walking uphill, the abdominal muscles will be more active than when walking on the plain.
The rectus abdominis muscles, when flexing and extending the spine, are antagonists of the group of paravertebral muscles, especially the latissimus dorsi, and are synergists with the iliopsoas muscle, acting together during flexion of the lumbosacral region.
Stretching
A sprain appears due to muscle overstrain, which happens when the load is greater than permissible, since the muscle corset is not sufficiently developed. With a strong increase in intra-abdominal pressure, a rupture of the abdominal wall is likely, which leads to displacement of organs (hernia), this often happens when lifting weights.
Tissue stretching is caused by strong contraction, which happens during flexibility training, turning, falling, or abdominal injury.
Microtraumas and muscle strains provoke spasms, which leads to pain. There are 3 degrees of severity:
- moderate (pain is not intense, goes away after 3–5 days);
- average;
- rupture (appears due to excessive pressure on the rectus abdominis muscles).
When the muscles are stretched, they need rest; it is recommended to avoid stress and sudden turns for at least two days. A cold compress will reduce pain. For severe pain, analgesics and anti-inflammatory drugs are prescribed. People often ask if muscles can ache for a week after an intense workout. When muscle tissue ruptures, pain lasts for more than 1.5 months.
Innervation of the rectus abdominis muscle
The rectus abdominis muscle is innervated by 7-12 intercostal nerves, originating from the corresponding spinal nerves. The muscle fibers between the different tendon bridges are innervated by the nerves of different segments, especially in the upper half of this muscle.
Inside the rectus abdominis muscle or in its transverse sheath, compression of the anterior branch of the spinal nerve can occur, thereby provoking true rectus abdominis syndrome, which is characterized by pain in the lower abdomen or pelvic area, simulating a gynecological disease in women.
Diagnostics
Differential diagnosis of diseases caused by trigger points in the abdominal muscle wall should take into account diseases such as:
- joint diseases,
- fibromyalgia,
- appendicitis,
- stomach ulcer,
- cholelithiasis with colic,
- colitis,
- diseases of the urinary system,
- menstrual irregularities,
- chronic pain in the pelvic cavity
- and other diseases.
When examining a patient, it is very important to pay serious attention to the patient’s posture when walking, standing and sitting.
Anamnestic data can help identify the cause of complaints of pain. The doctor draws up an accurate pain distribution diagram based on the patient’s words.
Myofascial trigger points of the rectus abdominis muscle depress its supporting function. If they are present in the rectus abdominis muscle, the patient's stomach sag when standing. A tight cord is felt throughout the abdomen, which is associated with an active trigger point, shortening only one segment of the muscle between the transverse tendon bridges in which it is located.
An active myofascial trigger point inhibits the contraction of adjacent segments of the rectus abdominis muscle. Contraction would help relieve tension in the affected muscle fibers, lengthening, rather than shortening the entire muscle as a whole. When taking deep breaths, the patient exhibits paradoxical breathing. While during quiet breathing exhalation is carried out due to the elasticity of the lungs and less assistance from the muscles is required, patients will subconsciously restrain the normal contraction of the diaphragm during inhalation, due to fear of pain when stretching the rectus abdominis muscle. This is a reflex inhibition of the muscles - the diaphragm and rectus abdominis.
And at the moment when the patient takes a deep breath with the participation of the diaphragm and thereby causes a protrusion of the abdomen, the pain reflected from the trigger points sharply worsens.
If there are trigger points in the rectus abdominis muscle, referred pain may be distributed along both sides of the spine, across the lower back. With deep breathing, the pain always intensifies, in particular when the back is straightened in the presence of pronounced lumbar lordosis, which subsequently causes stretching of the rectus abdominis muscle. Back pain caused by trigger points of the paravertebral muscles does not always affect the act of breathing. A hernial formation in the abdominal cavity is detected with the patient standing.
Symptoms caused by trigger points located in the abdominal muscles
Difficult-to-explain abdominal pain can often cause diagnostic confusion.
Referred pain caused by myofascial trigger points located in the abdominal muscles and somatovisceral effects can mimic diseases of the internal organs and systems.
In another case, on the contrary, with diseases of internal organs and systems, there is a profound impact on the sensitive somatic system of reflex activity. At the same time, active myofascial trigger points are aggravated, which causes the persistence of pain and other symptoms for a long time, even after the patient has recovered from the initial disease.
Active myofascial trigger points, localized in the abdominal muscles, for example, in the rectus muscle, can cause conditions such as: difficult muscle contraction, with the inability to “pull in” the stomach, relaxation, bloating. It is important to differentiate this condition from ascites.
Referred pain in the right upper quadrant can be caused by trigger points located along the outer edge of the rectus abdominis muscle. They can mimic the pain that accompanies gallbladder disease.
Referred pain simulating appendicitis may be projected from trigger points located in the lateral border of the rectus abdominis muscle and in the right lower quadrant.
Treatment of nervous tics
Mainly, the doctor examines the human body in order to exclude internal pathologies. The diagnosis is established after receiving the results of the study:
general blood test;
- blood biochemistry;
- MRI of the brain, spine;
- radiography;
- Electroencephalograms.
Consultation with a traumatologist, oncologist, psychiatrist, cardiologist, endocrinologist, etc. is also necessary.
Comprehensive treatment is undertaken:
- Taking sedatives to relieve tension in the nervous system.
- A certain daily routine in which rest and relaxation must be present.
- Massage course - up to 10 sessions. Manipulations that relax the nerve endings are carried out in the place where the muscle contraction occurs.
Massage helps to cope with nervous tics in the stomach
Alternative treatment
Surgery. For complex tics that interfere with the quality of life, doctors suggest a surgical method. In most cases, the problem is eliminated completely or partially. The surgeon tears the muscle, which undergoes constant contraction.
Botox. Botulinum toxin is a nerve poison and its injection into a muscle causes an immediate spasm that lasts up to six months, a year or more.
Unconventional methods for treating hyperkinesis
Recently, a technique has emerged that allows you to forget forever about almost all types of tics - vocal, motor, facial. How true this is is unknown. The method is called the “trance-impulsive method for nervous tics,” reviews of which are mixed. According to specialists of this technique, treatment is based on restoring the relationships between muscle structures. They are affected by negative charges that penetrate nerve endings caused by fears, fears, stress, anxieties, etc. The studied impulses are able to interrupt the invasion of negative particles and relieve the disorder.
Activation and long-term existence of myofascial trigger points
The reason for the long-term existence of myofascial trigger points can be structural and systemic factors, as well as posture and physical activity that are not corrected in a timely manner.
Muscles that are acutely or chronically overused can cause trigger points. Severe injuries, diseases of internal organs, emotional stress, as well as mechanical and toxic stress can cause the development of myofascial trigger points.
The location of active myofascial trigger points of the rectus abdominis muscle is usually the angle between the xiphoid process and the costal arch or between the umbilicus and the xiphoid process. In addition, trigger points can be located in the middle or lower part of the rectus abdominis muscle, along its lateral edge and in the area where the muscle attaches to the pubic bone.
Releasing Myafascial Trigger Points
Release from myafascial trigger points is facilitated by post-isometric relaxation, methods of contraction and relaxation, methods of cooling and stretching the abdominal muscles. The release method using fingertip pressure on a painful trigger point is only applicable to the superficial external rectus abdominis muscle. To treat myofascial trigger points at the insertions of the abdominal muscles, it becomes necessary to inactivate the central trigger point that causes them.
Corrective Actions
The persistence of the activity of the myofascial trigger point for a long time after the onset of an acute disease of the internal organ is facilitated by the fact that the initial cause, that is, the underlying disease - a tumor, stomach ulcer, intestinal paresis - has not been eliminated. Therefore, treatment aimed at getting rid of myofascial trigger points will give a temporary, partial effect. For a complete cure, it is necessary to eliminate the causative factor - a disease of the internal organ.
When a muscle remains in a stressful state for a long time, such as: emotional stress, viral disease, mechanical distortion, poor posture, stoop, it is also important to eliminate the cause that does not contribute to healing.
The patient should place a small pillow on the chair to support the lower back and sit leaning back in the chair. In this position, the lumbar lordosis increases, the chest rises slightly, and the longitudinal muscle fibers of the abdominal wall stretch.
It is necessary to avoid wearing a tight belt in order to improve blood circulation in the muscles.
Physical exercise
It is important to regularly perform special exercises for a long time to maintain normal muscle tone and form the correct pattern of movements.
The patient needs to perform therapeutic exercises, consisting of exercises to strengthen the abdominal muscles, aimed at developing diaphragmatic breathing and eliminating pelvic distortion.
All rights reserved by copyright law. No part of the contents of the site may be used, reproduced, transmitted by any electronic, copying or other means without the prior written permission of the copyright owner.
source
What else will help make your stomach flat?
As a basis for losing weight, many representatives of the fair sex choose strict diets with a minimum amount of calories. Torment by hunger with excessive physical exertion (training in the gym) gives a temporary effect.
When placed in extreme conditions, the body initially loses some weight, then turns on the energy-saving system, trying to create reserves for the time of forced hunger. The result of short-term or long-term self-torture is temporary weight loss and almost instantaneous weight gain.
One of the important reasons for the appearance of excess body weight is considered to be a hereditary predisposition to obesity.
Other sources of high weight are associated with:
- with physical inactivity – insufficient or absent physical and motor activity;
- an incorrectly selected diet - a predominance of light carbohydrates and large amounts of fat in the menu;
- consumption of alcoholic and low-alcohol tobacco products;
- environmental conditions;
- frequent stress;
- problems with the functioning of the intestinal tract.
Exercises for the lower abdomen will not give the desired result without an integrated approach. After identifying the source of rapid weight gain, you need to select a program for further action.
It includes various activities:
- consultation with a gastroenterologist – in case of digestive disorders, to normalize the functionality of the gastrointestinal tract;
- quitting smoking and drinking alcohol;
- selection of a suitable diet with calculation of the energy value of dishes;
- search for auxiliary types of therapy: massage sessions, water procedures, sports training.
Proper nutrition is very important to increase muscle strength. Eat healthy fats, proteins, complex carbohydrates, fruits and vegetables. Rev up your metabolism by eating 5 to 6 small meals a day. Add HIIT to your workout plan. This will increase the fat burning process. You can also start doing gymnastics. But always remember that without strength training you will never achieve a flat stomach.
All of the above exercises definitely guarantee excellent results. Try to focus on activating your core muscles. Research from the University of Hull states that if you mentally focus on your muscles and their movement, you can generate more muscle activity.
Head and neck
Pattern of referred pain and localization of trigger points in the upper part of the trapezius muscle. Solid red shows the main pain zone, grainy red shows possible additional zones.
The picture of referred pain and the localization of the trigger points responsible for it in the right sternocleidomastoid muscle. On the left is the sternal (superficial) portion. On the right is the clavicular (deep) portion.
Localization of trigger points in different parts of the masticatory muscle. Solid red shows the main pain zone, grainy red shows possible additional zones. On the left - the superficial layer, the upper and middle sections. In the center is the surface layer, the lower section. On the right is the deep layer, the upper part, just below the temporomandibular joint.
Picture of reflected pain from trigger points in the left temporal muscle. Solid red shows the main pain zone, grainy red shows possible additional zones. The anterior “spoke” of pain arises from the anterior fibers (TT1), the middle “spokes” from TT2 and TT3, the posterior (supra) “spoke” from TT4.
Medial hyoid muscle
A picture of referred pain (marked in red) and the location of the trigger points responsible for it in the medial hyoid muscle. On the left is the area of external pain that patients can point to. On the right is a picture of the internal part of the pain passing through the temporomandibular joint.
Lateral hyoid muscle
Pattern of referred pain from trigger points in the lateral hyoid muscle.
Picture of trigger points and pain reflected from them in the right digastric muscle.
On the left is the posterior abdomen - lateral view. On the right is the anterior abdomen - front view.
A picture of referred pain and trigger points in the right suboccipital muscle.
Pattern of referred pain (marked in red) and location of trigger points in the semispinalis muscles. On the left is the upper trigger point in the semispinalis capitis muscle. On the right is a trigger point in the third layer of the semispinalis muscle of the neck.
Trigger points and the pattern of pain they cause in the right splenius muscle of the head and neck. In the left pictures there are trigger points in the splenius muscles of the head, in the occipital triangle. In the right pictures there is an upper trigger point that causes pain in the eye orbits, a lower trigger point that causes pain in the angle of the neck.
Solid red shows the main pain zone, grainy red shows possible additional zones.
Shoulders, chest and arms
Referred pain and localization of TT2 in the upper part of the trapezius muscle, TT3, TT4 in the lower part, TT5, TTb in the middle parts of the trapezius muscle.
Levator scapulae muscle
A picture of mixed pain caused by two trigger points located in the right levator scapulae muscle. Solid red shows the main pain zone, grainy red shows possible additional zones.
A complex pattern of pain caused by trigger points located in the anterior, middle and posterior scalene muscles. Some trigger points may only have one persistent area of referred pain.
IPicture of referred pain and localization of trigger points in the pectoralis major muscle.
In the leftmost picture you can see how the pain reflected from two trigger points located in the middle part of the muscle near the sternum overlaps. The following figures show: on the left - a trigger point in the intermediate part of the sternum, in the center - the TT in the clavicular part, on the right - a trigger point in the area of the free edge of the muscle that forms the armpit.
Trigger point in the right pectoralis minor muscle and the pattern of pain it causes.
Picture of referred pain caused by a trigger point in the left pectoral muscle.
Picture of referred pain caused by a trigger point in the right subclavian muscle.
A pattern of referred pain caused by a trigger point located in the right serratus anterior muscle. Side, back and front views.
Serratus posterior superior muscle
A picture of referred pain from trigger points in the right posterior superior serratus muscle. Areas of constant pain are marked in solid red. Areas of possible pain are marked with grain. The left picture shows the rear view. In the figure in the center, the scapula is retracted forward and the trigger point becomes accessible for palpation and injection. The picture on the right is a front view.
Serratus posterior inferior muscle
A pattern of referred pain from trigger points in the right posterior inferior serratus muscle.
Pattern of referred pain and trigger points in the right latissimus dorsi muscle. The picture on the left shows the usual localization of a trigger point in the axillary portion of the muscle. In the center is the front view. On the right is a picture of pain from the lower trigger point.
Picture of referred pain and localization of trigger points in the right supraspinatus muscle.
The pattern of referred pain and the localization of trigger points in the right infraspinatus muscle.
The pattern of referred pain and the localization of the trigger point in the right teres minor muscle.
Medial and lateral (posterior and axillary) trigger points in the right teres major muscle and the pattern of pain reflected from them. On the left is the medial trigger point, on the right is the lateral TT.
|Picture of referred pain from trigger points in the right subscapularis muscle.
General picture of pain from trigger points in the right rhomboid muscle.
Pattern of referred pain and localization of trigger points in the right deltoid muscle. On the left is a picture of pain from trigger points in the anterior part of the muscle. The right pictures show a picture of pain from points in the posterior regions.
Pattern of pain and localization of trigger points in the right coracobrachialis muscle. Trigger points can be found in the distal or medial portion of the muscle. Sometimes the pain from them spreads only to the elbow.
Pattern of referred pain and localization of trigger points in the biceps brachii muscle.
Pattern of referred pain and localization of trigger points in the right brachial muscle. Note that the most superior trigger point may cause compression of the radial nerve.
Picture of referred pain and localization of trigger points in the triceps brachii muscle. On the left - TT1 in the left long head, TT2 in the lateral portion of the right middle head. In the center - TT3 in the lateral edge of the lateral head, TT4 deep in the distal part of the right middle head, in the center. On the right -TT5 deep in the medial edge of the right medial head.
Forearms and hands
Localization of trigger points in the elbow muscle and the pattern of pain reflected from them.
Pattern of referred pain and localization of trigger points in the three main extensors of the hand on the right side.
Localization of trigger points in the right brachioradialis muscle and the pattern of pain reflected from them.
Picture of referred pain and localization of trigger points in three selected muscles - finger extensors on the right hand.
Localization of the trigger point in the right arch support of the hand and the pattern of pain reflected from it.
Composite picture of referred pain and localization of trigger points in the right flexors of the hand and fingers.
Picture of referred pain and localization of trigger points in two muscles of the thumb of the right hand.
Picture of referred pain and localization of trigger points in the interosseous muscles of the right hand. Trigger points can be found in any part of the interosseous spaces. Sometimes they are called Heberden's nodes.
Back and stomach
Superficial paraspinal muscles
Insertion and location of the two most important superficial groups of paraspinal muscles (erector spinae).
The pattern of referred pain and the localization of trigger points in the pectoral iliocostal muscle.
The pattern of referred pain and the localization of trigger points in the lower thoracic and lumbar regions. Latin letters C, T, L, S and numbers indicate the levels of the vertebrae of the corresponding departments.
The pattern of referred pain and the localization of trigger points in the deep paravertebral muscles (multifidus and rotator cuffs). On the left is an example of trigger points in the midthoracic and lower sacral regions. In the center and on the right is the localization of TT in these muscles at the level of the L2 and S1 vertebrae.
Attachment and location of deep paraspinal muscles.
Multifidus muscles of the neck
The pattern of referred pain and the localization of trigger points in the deep muscles of the neck. Sometimes these points can cause compression of the greater occipital nerve.
The pattern of referred pain and the localization of trigger points in the right iliopsoas muscle.
A pattern of referred pain and visceral symptoms from trigger points located in the oblique abdominal muscles (and possibly the transverse muscle). On the left - “heartburn” due to a trigger point in the external oblique muscle, which attaches to the anterior chest wall. On the right - pain in the groin and/or scrotum due to a trigger point in the muscles of the lower-lateral abdominal wall.
Referred pain pattern and visceral symptoms due to trigger points in the rectus abdominis muscle. Left and center - bilateral pain throughout the back, fullness in the abdomen, nausea, vomiting can be caused by trigger points in the upper part of the rectus muscle. Similar bilateral pain in the lower regions can be caused by points in zone 2.
What actions are used in treatment
Treatment of the disease directly depends on the intensity and severity of the symptoms and the extent of the injury. So, with different degrees of severity, it can last from several days to several months.
The main thing for patients with this injury is to ensure complete rest for the abdominal muscles and the absence of any, even the most minimal, loads. In everyday life, you should avoid lifting heavy objects, sudden movements and other actions that cause contraction of the abdominal muscles. A gentle regimen is especially important in the first two days after the incident.
For moderate and severe sprains, it is recommended to apply cold in sessions of 15-20 minutes with breaks. Cold compresses will help reduce pain. As cold, you can use compresses made from ice cubes wrapped in cellophane and a towel. Applying ice directly to exposed skin is not recommended.
To relieve severe and intense pain, the doctor may prescribe anti-inflammatory drugs and analgesics in the form of tablets, injections or ointments. This will help significantly alleviate the condition and general well-being of the patient.
When the pain goes away, you can begin to gradually stretch the affected muscle. To do this, you can perform the most gentle exercises
, gradually complicating them and increasing the load.
In some cases, patients with these problems have to turn to modern plastic surgery. In this case, problems of an aesthetic nature are eliminated to a greater extent.
Pelvis, buttocks and thighs.
Quadratus lumborum muscle
Pattern of referred pain and trigger points in the quadratus lumborum muscle.
Trigger points are indicated to the left and center, which can be palpated just below the 12th rib and just above the ilium. On the right are trigger points in the deep layers of the muscle.
Anal sphincter, levator ani muscle, coccygeus muscle
Obturator internus muscle
The pattern of referred pain and trigger points in the pelvic floor muscles.
Pattern of referred pain and trigger points in the gluteus maximus muscle. Trigger points are localized: on the left (TT1) superomedial portion of the muscle. In the center (TT2) is a point in the area of the ischial tuberosity. On the right is the most medial inferior portion (MLP).
A picture of referred pain from trigger points in the injurious gluteal muscle.
Medial points (TT1) reflect pain in the iliac crest, in the sacroiliac joint and sacrum. TT2 are located slightly superior and lateral and refer pain lower to the buttocks. TTZ reflects bilateral pain in the sacrum and lower lumbar region.
The pictures show a picture of reflected pain from trigger points in the anterior portion of the right gluteus minimus muscle.
Additional zones appear when the muscle is fully engaged in work. In the right pictures there are points in the anterior portion of the muscle.
General picture of pain from trigger points in the right piriformis muscle. The most common lateral points (TT1)
Hip and knees
Tensor fascia lata
A pattern of referred pain from trigger points in the right tensor fascia lata muscle. The fascia in the figure has been removed.
Referred pain from three trigger points in the right sartorius muscle, located at different levels. Anterolateral view. Trigger points in this long muscle are located superficially, sometimes just under the skin.
B Picture of referred pain from trigger points in the right pectineus muscle.
Quadriceps femoris
Pattern of referred pain from trigger points in the right rectus femoris muscle.
A pattern of referred pain from trigger points in the right vastus medialis muscle.
A pattern of referred pain from trigger points in the right vastus medialis muscle.
There may be additional trigger points in the distal areas.
Anterior view of the right hip adductor muscles. A picture of reflected pain from trigger points located in these muscles.
Pattern of referred pain from trigger points in the right vastus lateralis muscle. The rectus femoris muscle is also shown.
TT1 points can block the movement of the patella. TT4 “closes” the fascia lata of the thigh and causes sharp pain, preventing sleep on the affected side.
Anterolateral view of the general pattern of pain referred from trigger points in the right gracilis muscle.
A pattern of referred pain from trigger points in the right hip adductor major muscle.
On the left is a front view. The center shows pain inside the pelvis caused by points in the TT2 area. These points lie deep and are sometimes located under the gluteus maximus muscles. On the right is an anatomical drawing.
Hamstring muscles
A picture of referred pain from trigger points in the muscles of the back of the thigh.
Pattern of referred pain from trigger points in the right right hamstring muscle
It must be remembered that this area contains large arteries, veins and nerves that may be affected.